Cinryze (human C1 esterase inhibitor) for hereditary angioedema
What is Cinryze for hereditary angioedema?
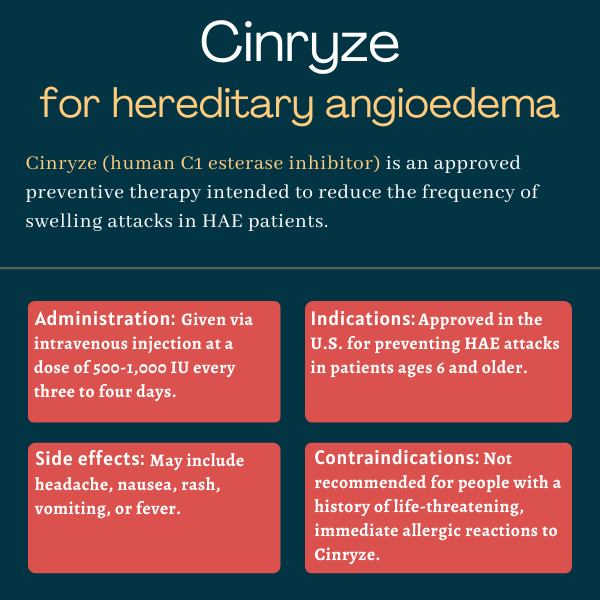
Cinryze (human C1 esterase inhibitor) is an approved treatment for children and adults with hereditary angioedema (HAE) that’s used to prevent sudden swelling attacks, the cardinal symptom of the disease.
Lev Pharmaceuticals originally developed and earned marketing authorization for Cinryze. The company later was acquired by ViroPharma, which was acquired by Shire in 2013. Shire is now a part of Takeda Pharmaceuticals, which markets Cinryze.
Cinryze is administered via an intravenous (into-the-vein) injection.
Therapy snapshot
| Brand name: | Cinryze |
| Chemical name: | C1 esterase inhibitor (human) |
| Usage: | Routine prevention of acute HAE attacks |
| Administration: | Intravenous injection |
How does Cinryze work?
In HAE, sudden swelling attacks are caused by the accumulation of a molecule called bradykinin. C1 esterase inhibitor, or C1-INH, is a protein that’s involved in controlling bradykinin production. People with the most common types of HAE have genetic mutations that lead to lower-than-normal C1-INH levels or activity, and excessive production of bradykinin.
Cinryze contains a version of C1-INH extracted from the blood of healthy donors. It works to replenish C1-INH levels in HAE patients, thereby preventing HAE attacks.
Who can take Cinryze?
Cinryze initially was approved by the U.S. Food and Drug Administration (FDA) in October 2008 to prevent HAE attacks in adolescents and adults, becoming the country’s first C1 esterase inhibitor for routine prophylaxis of HAE attacks. In June 2018, the FDA cleared a label expansion extending the use of Cinryze to children with HAE, ages 6 and older.
In the European Union, Cinryze is approved for the prevention of HAE attacks in patients ages 6 and older who have a history of severe attacks not managed by other treatments or who poorly tolerate other treatments. In Europe, the therapy also can be used in patients ages 2 and older to treat and prevent attacks occurring around the time of surgery or other medical procedures.
Who should not take Cinryze?
Cinryze is contraindicated, or not recommended, for patients who previously had life-threatening and immediate allergic reactions, including airway closure (anaphylaxis), to Cinryze.
How is Cinryze administered?
Cinryze is administered as an intravenous injection every three or four days. The medication comes as a freeze-dried powder in single use vials containing 500 international units (IUs) of C1-INH that must be reconstituted, or diluted, in a provided vial of sterile water (5 mL) prior to administration.
The dosage and infusion rate depend on a patient’s age:
- Ages 12 and older: Recommended dose of 1,000 IU, achieved by mixing two vials of Cinryze with two vials of water. Medication should be infused at a rate of 1 mL/minute over 10 minutes. Doses of up to 2,000 IU, but not exceeding 80 IU per kilogram of body weight, may be considered based on individual patient response.
- Ages 6-11: Recommended dose of 500 IU, achieved by mixing one vial of Cinryze with one vial of water. Infusion rate should be 1 mL/minute over five minutes. Doses of up to 1,000 IU may be considered based on individual responses.
A Mix2Vial transfer system is provided for reconstitution. After mixing, the solution will be colorless to slightly blue in color, and should not have any floating particles. It should be infused at room temperature within three hours of reconstitution and should never be frozen. Prior to reconstitution, the freeze-dried powder should be protected from light.
With proper training, patients and caregivers may be able to administer the medication. Otherwise, the injections need to be given by a healthcare provider.
Cinryze in clinical trials
The initial approval of Cinryze as a preventive therapy largely was supported by a Phase 3 trial (NCT01005888) that enrolled 24 HAE patients, ages 9 to 73, who were experiencing at least two attacks per month. The therapy’s label expansion to children as young as 6 in the U.S. was supported by data from a Phase 3 trial (NCT02052141) that enrolled 12 pediatric HAE patients, ages 7-11.
Preventive treatment
Participants in the Phase 3 trial that supported Cinryze’s initial approval as a prophylactic treatment were randomly assigned to receive Cinryze (1,000 IU) or a placebo every three to four days (approximately twice each week) for 12 weeks. This was followed by another 12-week period where those initially assigned to Cinryze switched to a placebo and vice versa.
Results showed that most patients experienced fewer attacks while on Cinryze than while on a placebo. Overall, the mean number of attacks over a 12-week period was 6.1 on Cinryze and 12.7 on placebo. Cinryze was associated with a 66% reduction in the number of days with swelling while on treatment compared with a placebo — 10.1 days versus 29.6 days. The therapy also was associated with significant decreases in average attack severity and duration.
An open label extension study called CHANGE 3 (NCT00462709) then evaluated the long-term use of Cinryze as a preventive HAE therapy. It enrolled 146 people, some from the earlier placebo-controlled trial and others newly recruited, all of whom were treated with Cinryze.
With treatment, most participants had a median HAE attack rate of less than one per month, compared with a median of three prior to enrolling in the trial. About one-third of patients (35%) reported no attacks during the study.
On-demand treatment
Another Phase 3 clinical trial (NCT00289211) assessed Cinryze’s safety and efficacy as an on-demand treatment of HAE attacks that did not involve the airways. In the main trial, 71 participants who reported to the clinic during an attack were randomly assigned to treatment with Cinryze (1,000 IU) or given a placebo.
Results showed that the median time to the onset of symptom relief with Cinryze was two hours, compared with more than four hours with a placebo. The median time to complete symptom resolution was 12.3 hours with Cinryze and 25 hours with a placebo.
The CHANGE 2 extension study (NCT00438815) evaluated Cinryze’s continued use as an on-demand treatment in patients, ages 1 and older. It enrolled 113 people, some of whom rolled over from the earlier trial. Across 609 total treated attacks, symptom relief started within an hour in 68% of the cases and within fours hours in 87%.
Pediatric patients
Among 46 children who were treated as part of the previous trials, 89% were found to experience relief from acute HAE symptoms within four hours of receiving Cinryze. When Cinryze was used as a preventive therapy, median monthly attack rates decreased from three to 0.39.
In another Phase 3 trial that backed Cinryze’s label expansion in the U.S., 12 children with HAE, ages 7-11, randomly received two doses of Cinryze (500 or 1,000 IU) for 12 weeks each.
Compared with previous rates, both doses of the therapy were associated with reductions in monthly HAE attack rates, which fell by a mean of 71.1% with the 500 IU dose and by 84.5% with the 1,000 IU dose. Mean monthly attack rates were 3.7 before the trial, dropping to 1.2 with the low dose and to 0.7 with the high dose. The severity of HAE attacks and the number of attacks requiring on-demand treatment also fell.
In a separate Phase 2 trial (NCT01095510), nine children, ages 2-11, received a single weight-based dose of Cinryze as a treatment for an acute attack. All experienced relief within four hours of receiving the medication.
Other trials
A Phase 2 clinical trial (NCT01095497) compared the safety and tolerability of under-the-skin (subcutaneous; 1,000 or 2,000 IU) and intravenous (1,000 IU) formulations of Cinryze in 26 HAE patients, each given twice a week for two weeks. Results showed that Cinryze was safe and tolerable with both administration methods, but the intravenous formulation was associated with fewer side effects, particularly injection-site reactions.
A Phase 4 study (NCT00914966) investigated the safety and tolerability of progressively increasing doses of Cinryze (1,500, 2,000, and 2,500 IU) in patients with uncontrolled HAE when receiving the treatment at its recommended dose. A total of 20 patients were enrolled and treated twice weekly for three months, starting at a dose of 1,500 IU dose. If HAE was not controlled after that period, the next highest dose would be given over another treatment period. If treatment was successful, participants continued at that dose over three months of follow-up.
Nine of the 20 patients achieved a treatment response, defined as an average monthly attack rate equal or inferior to one. These included four people at the 1,500 IU dose and five with 2,500 IU. Five of the 91 adverse events recorded during the entire study period were deemed to be related to Cinryze.
Common side effects of Cinryze
Common side effects associated with Cinryze include:
- headache
- nausea
- rash
- vomiting
- fever.
Allergic reactions
Allergic reactions to Cinryze are possible and could be life-threatening. Signs and symptoms may include hives, welts, chest tightness, wheezing, and low blood pressure, collectively known as anaphylaxis. Such reactions may be similar to HAE attacks, and treatments should be considered carefully.
Epinephrine, an injectable rescue medication for allergic reactions, should always be available to patients using Cinryze. If such a reaction occurs, Cinryze should be stopped immediately and appropriate treatment given.
Blood clots
Serious thromboembolic events, or blood clots, have been reported in HAE patients given C1-INH products, including Cinryze, at the recommended dose, as well as when used off-label at higher doses.
Risk factors for a blood clot may include an indwelling (inserted) catheter for repeated infusions, a history of blood clots, use of oral contraceptives or androgen medications, morbid obesity, and immobility. The potential benefits of Cinryze should be weighed against the risks of thromboembolic events for patients with underlying risk factors. If such patients are given Cinryze, they should be monitored during and after Cinryze infusions.
Transmission of infectious agents
Because Cinryze is made from human blood, it could contain infectious agents, such as viruses, and theoretically the Creutzfeldt-Jakob disease agent. All suspected infections should be reported by a patient’s healthcare provider to Takeda.
Use in pregnancy and breastfeeding
Adequate data are lacking to determine whether Cinryze may cause harm to a developing fetus. It should only be given to a pregnant woman if clearly needed.
Likewise, there are no data on the presence of Cinryze in human breast milk, or for its potential effects on a breastfed infant or on milk production. The benefits of breastfeeding should be considered along with the mother’s need for Cinryze and the potential adverse effects to the child.
Angioedema News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
 Fact-checked by
Fact-checked by