Angioedema triggered by anti-platelet medication ticagrelor: Report
Symptoms called usual because they came 20 days after treatment started
An elderly woman developed angioedema about 20 days after being given ticagrelor, a medicine that prevents blood clots from forming and is commonly used to lower the risk of a heart attack or stroke.
“Given the uncommon number of cases reported involving ticagrelor-induced angioedema and the even rarer, delayed onset case such as those described above, it is essential that clinicians are aware of this adverse effect,” the researchers wrote in “Ticagrelor: A Rare, Delayed Case of Angioedema,” which was published Cureus.
The woman’s status improved after she stopped ticagrelor and switched to the anti-platelet medication prasugrel.
“Both early detection and management modalities should be emphasized, and patients should be made aware of potential symptoms to facilitate timely identification and treatment,” the researchers wrote.
The combination of an anti-platelet agent, such as ticagrelor (sold as Brilinta, among other brand names), with aspirin is the mainstay treatment for managing some forms of heart disease and preventing thrombosis in patients who’ve had percutaneous coronary intervention, a minimally invasive procedure to open clogged arteries in the heart.
Known as dual antiplatelet therapy (DAPT), it uses medications that prevent platelets — tiny blood cell fragments involved in clotting — from sticking to each other and forming blood clots. Ticagrelor inhibits the platelet P2Y12 receptor.
While past reports described cases of angioedema triggered by clopidogrel, another anti-platelet agent sold as Plavix, limited evidence is available for hypersensitivity reactions associated with ticagrelor.
Physicians at the St Luke’s Hospital in the U.S. described the case of a patient who developed delayed-onset angioedema due to ticagrelor.
An uncommon reaction to ticagrelor
The patient, a 71-year-old woman, went to the hospital with chest pain that radiated to the left arm for the past two days. Blood work showed elevated levels of troponins, markers of heart damage. She had a past medical history of high blood pressure, high levels of fatty molecules in the blood, type 2 diabetes, and chronic kidney disease.
She was treated with 324 mg of aspirin, 90 mg of ticagrelor, and placed on a drip of heparin, an anti-coagulant. She had a narrowing (stenosis) of 80% in the mid-left descending heart artery, tests showed.
The woman had surgery to have a stent fitted to open up the artery and restore blood flow. She was then discharged on a daily DAPT regimen that included ticagrelor (90 mg) and aspirin (81 mg). She was also prescribed metoprolol succinate to control her high blood pressure.
Three weeks later she went to the emergency room with acute tongue swelling accompanied by difficulty speaking and an altered voice. She had no prior history of an allergic reaction to seafood, nor to aspirin or metoprolol succinate.
A medical examination confirmed her tongue was markedly swollen, nearly blocking her throat, although no respiratory compromise was seen.
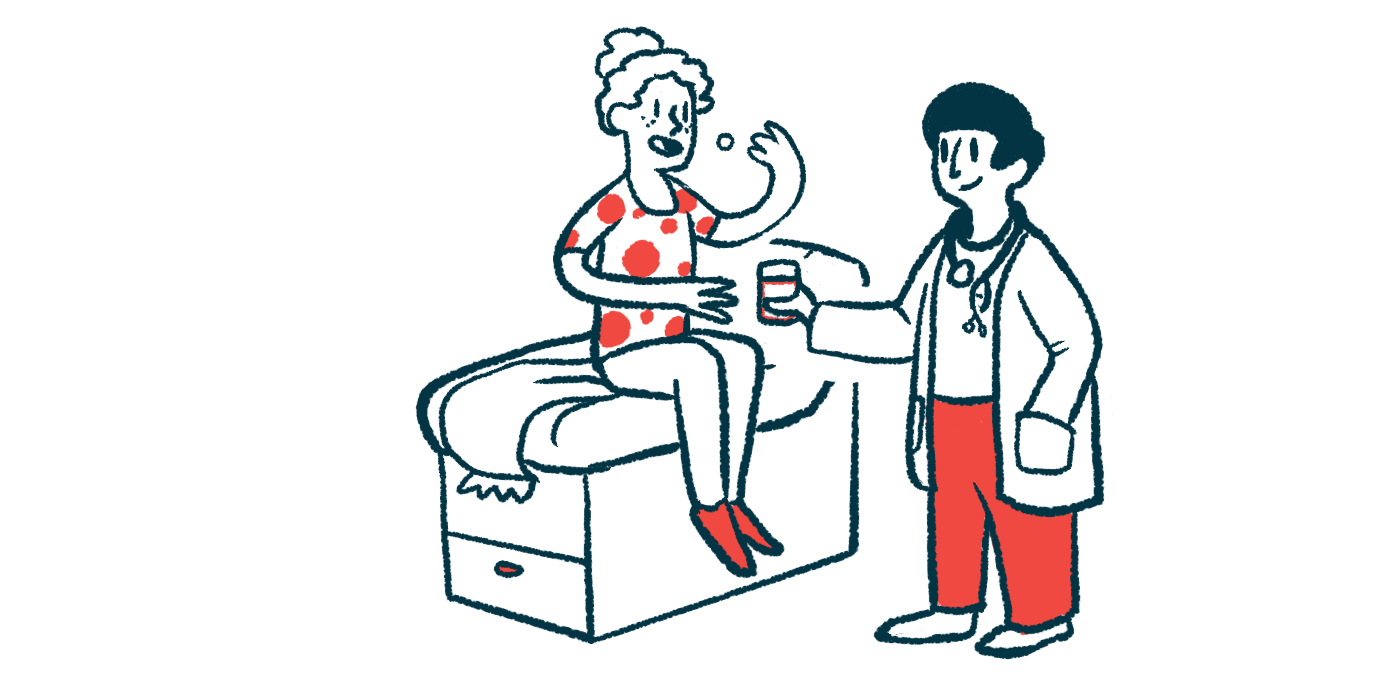
She received an intramuscular injection of epinephrine, a medication commonly used to treat severe allergic reactions, along with into-the-vein methylprednisolone, an anti-inflammatory, and diphenhydramine, an anti-histamine.
This led to a minimal improvement. She was transferred to the critical care unit for airway monitoring and began treatment with dexamethasone into the vein to reduce swelling.
After four dexamethasone doses, her tongue swelling eased and she was started on prasugrel, an anti-platelet medication sold as Effient. Blood work revealed no signs of acute angioedema and no symptoms or allergic reactions were observed with prasugrel. She was discharged with instructions to continue prasugrel (10mg) and aspirin (81 mg) daily.
The woman’s case was called unusual because her symptoms arose about 20 days after starting ticagrelor.
“The most delayed reaction reported in the literature occurred approximately 36 hours after the first dose of ticagrelor,” the researchers wrote. “The patient responded well to treatment with epinephrine, steroids, and antihistamines, and most importantly, discontinuation of the offending drug [ticagrelor]. The patient was promptly transitioned to prasugrel, a structurally dissimilar P2Y12 receptor inhibitor, without any interruption in DAPT.”